Telehealth flung open the doors to remote care, bridging geographical divides. Accessibility to healthcare services improved dramatically, reducing barriers from 65% to 90%. Yet, for many medical leaders, that initial promise feels… incomplete. Are your virtual visits straining under the weight of diagnostic ambiguity? Is valuable patient data from wearables creating noise rather than actionable insight? Are operational bottlenecks hindering the very access telemedicine was meant to expand? It often feels like connection without true adaptation, reaction without foresight.
Consider, instead, a healthcare delivery model that doesn’t just connect, but learns. A system architected to perceive subtle patient changes before they become critical, predict needs proactively, personalize interventions on the fly, and optimize its own workflows intelligently. This isn’t a far-off vision; it’s the Adaptive Clinic. Powered by the sophisticated capabilities of AI in telemedicine, this ecosystem constantly adapts, creating a truly responsive, efficient, and patient-centric experience.
As leaders navigating the relentless pressures of cost, competition, access, and outcomes, you know incremental improvements aren’t enough. Artificial intelligence offers the quantum leap. It’s not futuristic fantasy; it’s the core architectural cognition available today to fundamentally reshape telehealth. Consider this article your strategic roadmap – a guide to understanding and constructing the key AI-based telemedicine components that form the foundation of a truly Adaptive Clinic your patients will value, and your organization will thrive on.
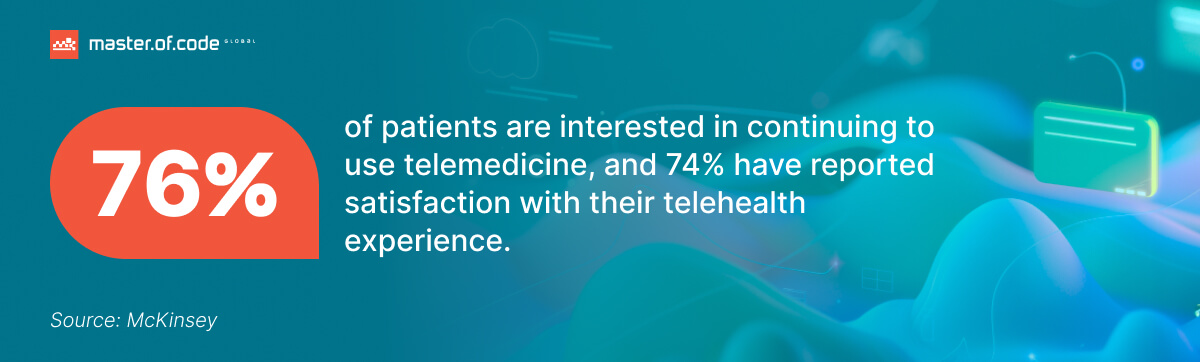
Table of Contents
The Core Blueprint: Key Applications of AI in Telemedicine
Building an Adaptive Clinic isn’t about adding a few digital bells and whistles; it’s about embedding intelligence into the very fabric of remote healthcare. Just as a master architect relies on foundational structures, specialized systems, and robust infrastructure, the facility is constructed from distinct yet interconnected capabilities. These applications of AI in telemedicine are the load-bearing walls, the intelligent wiring, and the adaptable frameworks that transform potential into performance. Let’s explore the essential components layer by layer, understanding how each contributes to a more perceptive, predictive, personalized, efficient, and accessible healthcare future.
Foundational Layer: Intelligent Perception – Visual AI Seeing and Hearing What Humans Might Miss
Every effective structure begins with a solid base. In the Adaptive Clinic, this foundation is built upon Intelligent Perception – the ability to accurately sense, interpret, and understand patient status remotely, often exceeding human limitations. This is where AI in telehealth dramatically enhances diagnostic accuracy and supports more timely interventions. Imagine a radiologist reviewing CT scans transmitted from a remote clinic; AI-assisted telemedicine can act as a tireless, expert assistant, flagging subtle anomalies indicative of early-stage disease that might otherwise be missed.
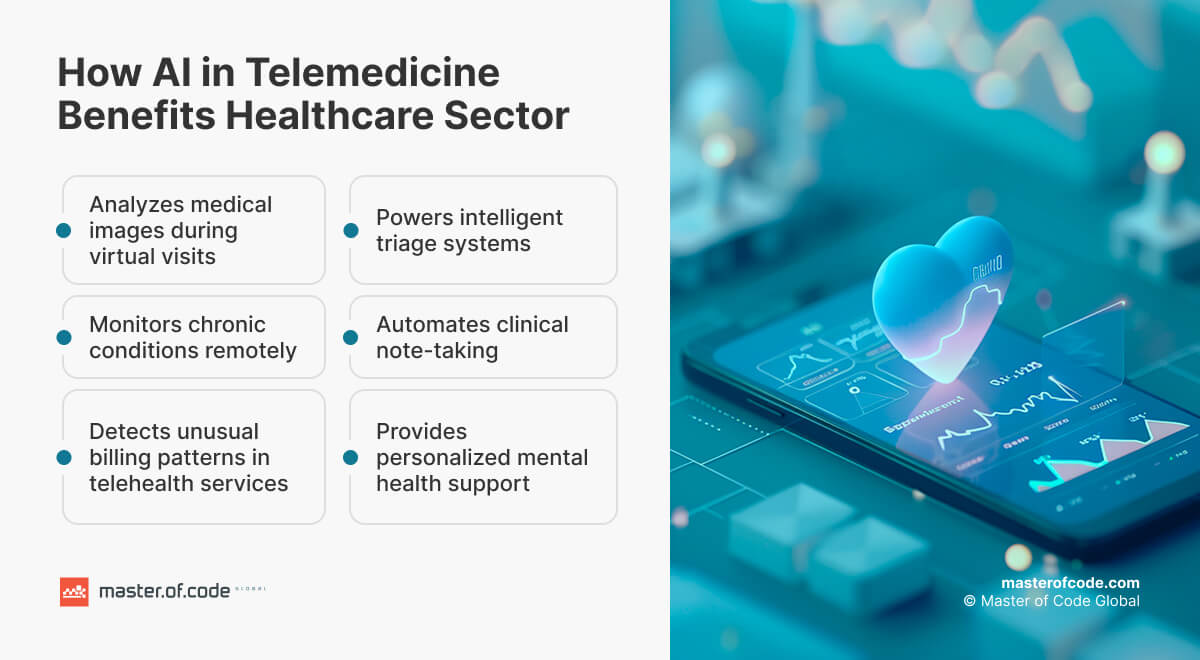
Consider dermatology consultations via telehealth, where artificial intelligence analyzes medical images with remarkable precision, comparing them against vast datasets to assist in identifying potential malignancies. Or ophthalmology, where visual AI in telemedicine diagnostics screens retinal scans sent from primary care settings for signs of diabetic retinopathy, enabling sight-saving interventions sooner.
This intelligent perception extends directly into the virtual visit itself. AI in telehealth tools can analyze reported symptoms in real time, cross-referencing medical literature and patient data to suggest potential diagnoses or necessary tests. These systems act as sophisticated clinical decision support, even flagging possible drug interactions or contraindications based on one’s record – adding a crucial layer of safety.
Furthermore, real-time visual AI in telehealth is rapidly evolving beyond static imagery. Sophisticated algorithms can now assess gait and mobility via video, monitor the healing of wounds over time through photos, track physical therapy adherence, or even interpret non-verbal pain cues — all under strict ethical and consent standards. Briefly, visual AI in telehealth is also learning to examine audio and text: voice patterns for respiratory or neurological signs, and short-form messages for emergent health issues.
This foundational layer ensures the Adaptive Clinic operates on a richer, more accurate understanding of patient well-being, helping healthcare providers deliver care that is sharper, faster, and more proactive.
The Structural Core: Predictive Stability – Remote Patient Monitoring & Anticipating Health Trajectories
We build a reliable and forward-looking system on the foundation of perception, using consistent predictions. This is powered by AI in telehealth and its advanced role in remote patient monitoring. Healthcare organizations are increasingly awash in data streamed from wearables, sensors, and self-reporting tools – heart rate, blood pressure, glucose, oxygen saturation, activity levels, symptoms. The challenge isn’t collection, but transformation: turning this flood into actionable cognition.
This is where artificial intelligence in telemedicine becomes indispensable. Sophisticated algorithms sift through physiological indicators, learning individual patient baselines and identifying subtle deviations that flag impending trouble. This level of proactive monitoring is increasingly powered by virtual care models – approximately 80% of clients have received care through virtual channels, often leveraging data from wearables and self-reporting tools for prescription care and minor illness.
Instead of simply reporting a single high reading, artificial intelligence enables earlier interventions by detecting warning patterns – for instance, signs of worsening heart failure days in advance, or glycemic trends pointing toward diabetic ketoacidosis. This is AI predictive analytics in healthcare at its most impactful: acting as an embedded early warning system within the Adaptive Clinic’s core.
Imagine the real-world effect: a digital alert prompts a care manager to schedule a timely virtual visit for a patient whose vitals suggest early heart failure decompensation – leading to a medication tweak that prevents hospitalization. Or a high-risk diabetic recipient is flagged by AI-enabled telehealth systems, triggering automated education content and nurse follow-up. This proactive approach supports more effective disease management and improves overall patient outcomes.
The benefits are significant: fewer preventable hospitalizations, better chronic care, and smarter clinical resource allocation. It’s this remote monitoring–driven predictive stability that reinforces the Adaptive Clinic’s capacity to anticipate, not just react.
Custom Blueprints: Personalized Care – AI Designing Care for the Individual
With a stable, perceptive structure in place, the Adaptive Clinic distinguishes itself through personalized care. Standardized, one-size-fits-all protocols are becoming relics of the past. AI in telehealth now enables us to move toward truly tailored healthcare journeys, built from the ground up for each individual. Acting as the master designer, this technology analyzes layers of data – demographics, medical history, lifestyle patterns, genetic insights (where available and consented), and real-time metrics from remote patient monitoring devices – to architect smarter care plans.
This goes beyond stratification. Artificial intelligence makes real-time treatment recommendations based on risk and response patterns, helping healthcare providers fine-tune therapies, adjust medication dosages dynamically, or tailor follow-up timelines according to measurable progress. This level of adaptation, supported by AI-enabled telehealth, makes sure that care is both scientifically sound and deeply individualized.
Moreover, digital tools transform patient engagement. Portals within telemedicine chatbot systems can deliver content aligned to a person’s condition, stage, and behavior. Smart reminders are triggered by data trends – nudging medication adherence or prompting lifestyle interventions. AI can even assist in matching individuals to ideal specialists or help groups, based on current needs and preferences.
The result is transformative: improved satisfaction, increased adherence, and better overall patient outcomes. Resources are used more strategically, and every recipient’s journey becomes a reflection of who they are – not just what they have. This is the heart of truly personalized care in the Adaptive Clinic.
The Smart Infrastructure: Efficient Healthcare Operations – Optimizing the Flow of Care
No architectural marvel functions without an efficient framework. The Smart Infrastructure of the Adaptive Clinic uses AI in telemedicine to achieve operational autonomy – streamlining the administrative and logistical underpinnings of modern care delivery. This is where the backend of AI-enabled telehealth becomes not just efficient, but intelligent.
Consider the mountain of non-clinical tasks that consume time. Digital tools address this head-on. Scheduling systems optimize appointments based on urgency and provider availability. Artificial intelligence development solutions now automate bookings, eligibility checks, and documentation workflows with growing sophistication. Picture real-time prior authorization and easy claims processing – massively reducing friction and delays.
One of the most life-changing innovations is ambient clinical intelligence. During virtual consultations, AI listens unobtrusively and automatically generates notes, flags key diagnoses, and even suggests billing codes or referral options. This dramatically reduces documentation burden, boosting patient care time and lowering clinician burnout. Use of AI in electronic health records also makes sure these notes integrate seamlessly into your EMR ecosystem, strengthening workflow continuity.
For health systems navigating financial pressures, operational automation driven by digital results in tangible value—lower admin costs, better throughput, and a more agile revenue cycle. These improvements free up staff and tech to focus on their core purpose: delivering excellent, human-centered patient care.
Expanding the Footprint: Access to Healthcare in Underserved Areas
The true power of the Adaptive Clinic lies in its ability to erase limitations. Digital telemedicine isn’t just boosting existing workflows – it’s driving AI in telehealth toward new frontiers, creating more equitable and widespread care. Through smart automation, predictive intelligence, and scalable platforms, it’s enabling virtual healthcare to thrive even in low-resource or underserved areas.
How does it work? The capabilities we’ve discussed – improved diagnostics, predictive analytics, personalization, and automation – come together in the field. A community worker in a remote location might use a digital tool to screen for common health issues, triggering faster triage. RPM programs, guided by remote monitoring algorithms, allow city-based healthcare providers to manage chronic conditions like hypertension or diabetes from miles away.
AI guarantees specialist time is reserved for complex cases flagged by earlier evaluations. And in multilingual regions, automated translation tools within telehealth software remove language barriers. Combined, these capabilities enable telehealth to become a vehicle not just for basic check-ins, but for advanced diagnostics, remote chronic disease management, and tailored follow-up – even where infrastructure is minimal. In telepsychiatry practices, for example, artificial intelligence has also reduced the time required to complete session notes by 23%, allowing therapists to dedicate more time to patients.
The impact is massive: broader reach for specialists, optimized long-term condition oversight, more scalable public health efforts, and fewer gaps in care. Healthcare providers can finally serve rural and vulnerable populations with a level of depth and intelligence once thought impossible – transforming remote monitoring into a lifeline for quality services.
Future of AI in Telemedicine: Adding Intelligent Facades & Foresight
The Adaptive Clinic blueprint is just the beginning. As new technologies emerge, the architecture evolves, layering on more sophistication and intelligence. The most exciting developments lie in its digital features and predictive foresight.
Start with the transformation of the digital front door. Basic bots are now evolving into advanced AI-powered chatbots & AI agents – virtual health assistants that guide customers across their journey. These self-learning solutions, embedded in telemedicine tools, can handle symptom triage, intake, scheduling, education, and even ongoing care management. Always-on, responsive, and context-aware, they’re redefining how client engage with providers and deliver greater patient satisfaction.
At a system level, AI-driven predictive analytics in healthcare is making big leaps. While earlier models focused on individual risk, the new frontier involves large-scale predictions that impact entire domain. For example, the use of forecasting technology in hospitals has reduced the rate of readmissions from 23% to 10%.
Algorithms analyze population-level data, social trends, and environmental inputs to forecast disease outbreaks, manage ER surges, and inform public health strategy. This strategic layer turns artificial intelligence into a control tower for care delivery.
Other breakthroughs include AI for predictive maintenance of medical devices, offering uptime of essential hardware for virtual diagnostics, and greater integration with biometric streams that enable hyper-personalized recommendations in real time. New innovations in remote patient monitoring and behavioral tools are also making virtual mental care more scalable and adaptive.
Of course, organizations must weigh the cost of AI in healthcare, considering both implementation investment and long-term ROI. But with the right strategy and systems, these intelligent additions deliver value far beyond their initial spend – both operationally and in measurable patient outcomes.
Choosing Your Master Builder: Partnership in Digital Implementation
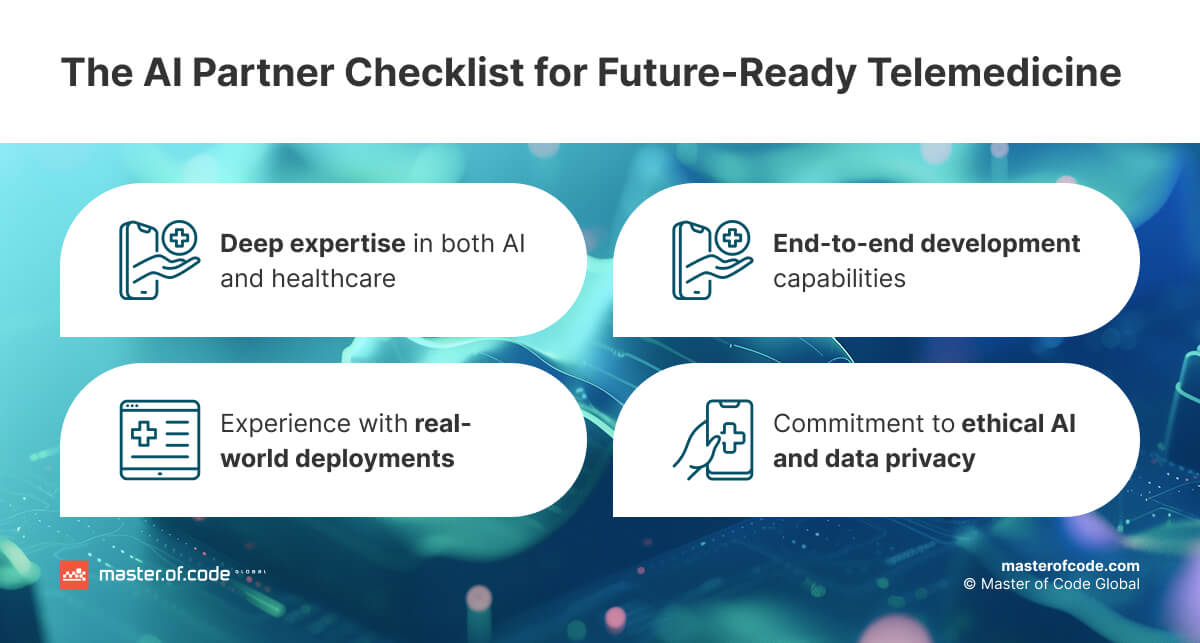
The vision of the Adaptive Clinic, powered by AI in telemedicine, holds immense promise. But realizing this vision requires more than technology – it calls for deep expertise and the right partnership. Implementing these systems means addressing critical challenges: system integration, workflow redesign, ethical use, regulatory compliance, and provider adoption.
That’s where expert AI healthcare consulting makes the difference. The right partner brings not only cutting-edge algorithmic capabilities, but also hands-on experience navigating the intricacies of medical systems. They help you align technology with your operational realities and clinical goals.
An ideal partner also understands how AI in health insurance intersects with virtual care delivery. From reimbursement models and claims optimization to proactive risk assessments, digital solutions must fit within the broader financing landscape. Choosing someone fluent in these nuances ensures not just technical success, but strategic alignment.
Finally, excellence isn’t measured by novelty – it’s measured by impact. The best healthcare professionals are those who select partners that can demonstrate measurable outcomes, be sure disease management strategies are scalable, and drive long-term value through intelligent systems designed for real-world complexity.
At Master of Code Global, we embody these very principles – and a prime example is our AI-powered Medication Management Platform. Designed to future-proof healthcare delivery, this intelligent solution goes far beyond traditional reminder apps. It acts as a comprehensive virtual medicine cabinet, helping users manage complex treatment schedules, avoid missed doses, and stay informed about their health. The platform integrates effortlessly into users’ daily routines, offering personalized support and real-time medication tracking. To date, it has securely processed over 1 million medication records with zero data breaches – demonstrating our commitment to both innovation and patient safety.
Architect’s Q&A: Answering Key Construction Queries
Q1: Where is AI making the biggest impact in telemedicine structures today?
The influence of AI in telemedicine is already widespread and growing. Currently, the most promising applications are significantly improving diagnostic accuracy, especially through sophisticated analysis of medical images during remote consultations. Beyond diagnostics, remote monitoring is enabling proactive care via predictive alerts. Administrative burden is also decreasing thanks to documentation workflows. Critically, artificial intelligence is empowering healthcare providers to deliver more tailored experiences, and it’s playing a vital role in expanding care access to underserved populations, making telemedicine smarter and more effective right now.
Q2: What innovative ‘smart materials’ and techniques are emerging for next-gen telehealth architecture?
Innovation in AI in telemedicine continues to accelerate. Today’s most advanced developments include conversational agents that act as full-service virtual assistants for patient triage, navigation, and engagement. In parallel, system-wide predictive analytics in healthcare offer deep insight into public health trends and resource needs. We’re also seeing progress in visual AI in telehealth, with real-time tools interpreting video data for physical therapy, wound assessment, and pain detection. These innovations are creating a more integrated, intelligent, and responsive care ecosystem.
Q3: Why lay the foundation now? What’s the structural integrity and ROI of building an intelligent telemedicine system?
Investing in a digital clinic is a present-day competitive imperative. The benefits of artificial intelligence in telehealth include earlier detection, proactive intervention, and smarter workflows. The returns are measurable: better patient outcomes, reduced burnout, lower costs, and increased operational agility. Moreover, it positions your organization to adapt quickly in a fast-changing healthcare landscape. The long-term strength of this foundation lies in building a care system that’s not just more connected, but more intelligent, adaptive, and resilient.
Laying the First Stone – Commission Your Adaptive Clinic
The blueprint is clear. An AI-powered clinic – capable of delivering truly responsive, predictive, personalized, and efficient care – represents the definitive future of telemedicine. This isn’t merely a theoretical possibility; it’s an achievable reality addressing the core challenges facing healthcare leaders like you today. By 2026, 25–30% of all medical visits are predicted to be conducted via telemedicine, with artificial intelligence playing a key role in analyzing patient data and improving diagnostics.
Realizing this game-changing vision, however, requires expert execution and the right strategic construction partner. Are you ready to move from blueprint to build? Let the experienced AI and healthcare architects at Master Of Code Global help you begin the journey.
Ready to build your own Conversational AI solution? Let’s chat!